- Aboutchevron_right
- About Terry Wahls
- The Wahls Protocol®chevron_right
- Cooking For Lifechevron_right
- Dr. Wahls Research Fund
- Clinical Trials
- About Terry Wahls
- Programschevron_right
- Media + Presschevron_right
- Resourceschevron_right
- Events
- Blog
- Shopchevron_right
Blog
Supplements for Autoimmune Health: Functional Medicine vs. Conventional Approaches

Your immune system is how your body fights off illness and heals itself. The foods you eat have a direct impact on your immune health. Adding certain foods to your diet supplies your body with the nutrients it needs to support immune cell production and function. Here are some of the best foods to support immune function that you should incorporate into your diet.
Supplements for Autoimmune Health: Functional Medicine vs. Conventional ApproachesMagnesium for MS and Beyond: Are You Missing This Vital Nutrient?

In this blog, I will be discussing all things magnesium — its role in maintaining your health, why your magnesium levels may become low, the symptoms associated with magnesium deficiency, and what you can do to optimize your magnesium levels.
Magnesium for MS and Beyond: Are You Missing This Vital Nutrient?Chronic Fatigue Starts in the Gut: How Microbes Impact Energy and Brain Health

In this article I will discuss the problem of fatigue in people with multiple sclerosis (MS) and other neurological disorders. I’ll share my personal experiences with fatigue, explain some of the underlying biological factors that contribute to fatigue, and highlight the essential role B vitamins play in supporting mitochondrial function.
Chronic Fatigue Starts in the Gut: How Microbes Impact Energy and Brain HealthMuscle Mass and MS: Preventing Sarcopenia with Diet, Exercise, and Hormone Support

I want you to thrive into your 70s, 80s, 90s, and beyond. Building and maintaining your muscle mass is crucial in helping you achieve that goal, and that’s what we’ll be discussing in this article.
Muscle Mass and MS: Preventing Sarcopenia with Diet, Exercise, and Hormone SupportIs Juicing Right for You? When It Helps, When It Harms, and How to Detox Safely

In this article I’ll explore the role juicing can play in detoxification; how to spot the signs that juicing may harming more than it’s helping; and sustainable food and supplement recommendations to support your long-term health (without the risks).
Is Juicing Right for You? When It Helps, When It Harms, and How to Detox SafelyWhy Is Nutrition Still So Controversial? Exploring the Pushback Against Healing Through Food

Why do so many people reject the idea that better nutrition and self-care could improve quality of life (and reduce the need for prescription medications) for people with MS and other chronic health conditions?
Why Is Nutrition Still So Controversial? Exploring the Pushback Against Healing Through FoodMS Patients: Here’s How to Relieve Your Pain without Damaging Your Gut

Today we’re going to examine the role of over the counter pain medications (like ibuprofen) that may relieve pain and inflammation, but can also increase your risk of intestinal permeability, also known as leaky gut. I will also point you to some herbal supplements that work through the same pathways to manage pain—without causing a leaky gut.
MS Patients: Here’s How to Relieve Your Pain without Damaging Your GutInflammasomes and MS: How NLRP3 Drives Neuroinflammation and What You Can Do About It

In this blog I will review a recent paper on the molecular mechanisms that drive disability progression in multiple sclerosis (MS), Alzheimer's, Parkinson’s, and many chronic disease states. I will also give specific recommendations to address those issues.
Inflammasomes and MS: How NLRP3 Drives Neuroinflammation and What You Can Do About ItHow Toxins Sabotage Your Health—And What to Do About It

We are exposed to toxins daily, in our homes, workplaces, and through the products we consume. Your body’s toxin burden refers to the total amount of harmful substances—like heavy metals, pesticides, or industrial chemicals—that are stored in your tissues (especially fat and bone).
How Toxins Sabotage Your Health—And What to Do About ItOverwhelmed by the Wahls Protocol? Start Here.

Enjoy this guest post from Wahls Protocol® Health Practitioner Alene Brennan
Overwhelmed by the Wahls Protocol? Start Here.The Supplements and Vitamins You Need to Support Healthy Bones and Prevent Osteoporosis

People with MS have higher rates of osteopenia, osteoporosis, falls and fractures.<sup>1</sup> In this article, we’ll look at why that is, how these conditions occur, and the impact they can have on quality of life. I will also share my recommendations and strategies around how to support stronger, healthier bones and live a full, healthy life.
The Supplements and Vitamins You Need to Support Healthy Bones and Prevent OsteoporosisWhy Minerals Are Important for People with Multiple Sclerosis (MS)

In this article, I will examine the importance of minerals for people with multiple sclerosis (MS); the declining mineral content in our food supply; signs that may suggest mineral deficiency; and how you can improve your mineral balance through diet and supplementation.
Why Minerals Are Important for People with Multiple Sclerosis (MS)What Supplements Should I Take for MS?

I am often asked what supplements I should take if I have multiple sclerosis (MS). In this blog, I’ll discuss the nutritional issues for people with MS and chronic health problems and my health journey, as well as provide a few suggestions for where to begin when it comes to what supplements you should take for MS.
What Supplements Should I Take for MS?What's the Best Diet to Control Multiple Sclerosis?

Which is the best diet for multiple sclerosis (MS) is one of the most common questions I get. Unfortunately, too many neurologists are stilling their patients that there is no research showing diet makes no difference for people with MS. They are wrong. I do clinical research testing the effects of diet in people with MS. Our studies have included the modified Paleolithic diet (also known as the Wahls™ diet), the ketogenic diet, and the low saturated fat diet (also known as the Swank diet).<sup>1-7</sup>
What's the Best Diet to Control Multiple Sclerosis?6 Reasons to Take Probiotic Supplements

Probiotics are live bacteria that offer many benefits for your gut and overall health. These microorganisms can be consumed in fermented foods, but many people benefit from taking probiotic supplements to add increased variety to your gut’s existing supply of friendly bacteria. Keep reading to learn some of the top reasons to take probiotic supplements and how they can improve your health.
6 Reasons to Take Probiotic Supplements7 Healthy Ways to Manage Stress

Stress can wreak havoc on your health. Chronic stress can cause digestive issues, sleep disturbances, weakened immune system, and worsened health conditions. If you want to reduce the effects of stress on your health, it’s important to find healthy ways to manage your stress. Here’s a list of some of the most effective ways to manage stress:
7 Healthy Ways to Manage Stress10 of the Best Foods to Support Immune Function

Your immune system is how your body fights off illness and heals itself. The foods you eat have a direct impact on your immune health. Adding certain foods to your diet supplies your body with the nutrients it needs to support immune cell production and function. Here are some of the best foods to support immune function that you should incorporate into your diet.
10 of the Best Foods to Support Immune FunctionDiscover How The Sense Of Smell Can Signal Safety To Your Body, Promoting Healing and Well-Being
![vbo-videographics2-scaled[1]](/media/66a0cb6a3a115e97b72c5b46/large.webp)
In this interview with Jodi Cohen from <a href="https://dv216.isrefer.com/go/VBO/DrTerryWahls/" target="_blank">Vibrant Blue Oils</a>, we delve into the concept of safety and how essential oils can help improve our sense of safety. When our bodies perceive a continuous threat, they redirect resources to escape rather than heal. Jodi and I explore how we can shift to a safer environment using essential oils.
Discover How The Sense Of Smell Can Signal Safety To Your Body, Promoting Healing and Well-BeingThe Essential Role of Phospholipids in Autoimmune Health
In a world where dietary trends fluctuate frequently, the importance of foundational nutrients remains constant. Among these, phospholipids stand out due to their crucial role in cellular health and overall well-being. Recently, Dr. Wahls, a staunch advocate for managing autoimmune conditions through diet, joined forces with Jess Kane from BodyBio to discuss the significance of these essential molecules.
The Essential Role of Phospholipids in Autoimmune HealthGet Involved in a Clinical Trial
I also encourage you to take part in a clinical trial. For many, being in a clinical trial provides additional motivation to make and sustain dietary improvements. Having one family member in a diet study often helps the whole family improve their diet. Consider being in one of our upcoming trials today.
Get Involved in a Clinical TrialFrom the Battlefield to Your Bowl: Captain Soup’s Healing Journey

From the Battlefield to Your Bowl: Captain Soup’s Healing Journey Discover How Military Veteran Turned Entrepreneur, Captain Soup, Revolutionized His Health and Created a Nutrient-Dense Soup Line to Support Healing Journeys Join me in an exclusive interview with Brian Gaudette, the visionary behind Captain Soup. Uncover the remarkable journey of how he battled health challenges as an army pilot and triumphed over autoimmune symptoms, leveraging the healing power of food.
From the Battlefield to Your Bowl: Captain Soup’s Healing JourneyCrucial ZZZs: How Quality Sleep Nourishes the Autoimmune System

How is your sleep? Ever since I was a teenager I have struggled with sleep. During college, medical school, and residency, I thought that sleeping 4-6 hours a night was an advantage. I had a lot of studying to do so I thought it was helpful to not sleep so much. Now I know better. Sleep is important for our mental health and our brain health. I will give a few tips for improving sleep and a link about a research study later in the article.
Crucial ZZZs: How Quality Sleep Nourishes the Autoimmune SystemThe Xenoestrogen Effect: How Synthetic Chemicals Impact Your Hormonal Health
Estrogen might be a problem for women and for men.[1-3] Could this be part of your health issues? If you are struggling with severe periods, heavy bleeding, intense menstrual cramps, and mood swings with your periods, you may have an excessive estrogen effect. Men can also be impacted. If you are having, having difficulty with low libido or difficulty achieving and maintaining erections, you may be having an excess estrogen effect.
The Xenoestrogen Effect: How Synthetic Chemicals Impact Your Hormonal HealthThe Endless Benefits of Sulfur-Rich Vegetables: Cancer Prevention, Detoxification, Gene Expression and more…

There is ample evidence of the health benefits of eating broccoli and other cabbage family vegetables. These foods contain glucoraphanin, which, in the right circumstances, is metabolized to sulforaphane, which is associated with many health benefits.
The Endless Benefits of Sulfur-Rich Vegetables: Cancer Prevention, Detoxification, Gene Expression and more…Fat: Friend or Foe for Multiple Sclerosis Patients?
The best answers come from studies that combine all the reported randomized controlled diet studies with MS patients that had fatigue or quality of life as an outcome. The consistent finding is that adopting certain diets lead to reduced fatigue and improved quality of life [1-3] and that eating more added sugars and highly processed foods lead to worse mental health outcomes [4]. Dr. Linda Snetselaar conducted a network meta-analysis of 12 diet studies in people with MS, comparing 8 diets with 608 total study participants.
Fat: Friend or Foe for Multiple Sclerosis Patients?Eat, Learn, Grow Healthy: Growing Strong – Our First Children’s Book

Eat, Learn, Grow Healthy: Growing Strong – Our First Children’s Book The Why Behind Writing A Children’s Book for All Our Children My sister died when I was 8 years old. In retrospect, I realize that was a particularly severe adverse childhood experience that had a profound impact on my life and contributed to my health challenges later in life. My daughter Zeb was 8 when I got my wheelchair. That was the onset of her severe adverse childhood experience. Years of watching the person who was supposed to be invincible growing steadily more frail each year. A profound adverse childhood experience. This affects many of our children.
Eat, Learn, Grow Healthy: Growing Strong – Our First Children’s BookWhen and how can you stop taking a disease-modifying treatment (DMT)?

As people age, their immune system becomes less and less effective at creating inflammation. There are fewer and fewer autoimmune flares of disease activity, meaning fewer relapses and fewer new, enhancing lesions but more infections and cancers that the immune system cannot overcome, leading to serious health decline. So when does continuing immune-suppressing DMTs outweigh the higher risk of infection and/or cancer? Neurologists and other specialists and their patients want guidance on how to address this question.
When and how can you stop taking a disease-modifying treatment (DMT)?How Ketogenic Diets Can Help Manage Autoimmune Conditions

People with autoimmune issues are at greater risk for elevated blood sugar and blood lipids than the general public. More people are using a ketogenic diet to improve blood sugar metabolism, and there are more and more research clinical trials examining the impact of a ketogenic diet on blood sugar metabolism and type-2 diabetes.
How Ketogenic Diets Can Help Manage Autoimmune ConditionsChanging The Standard Of Care

My big hairy audacious goal is to change the standard of care. I want all patients newly diagnosed with MS, autoimmune condition, or a complex chronic health problem that includes neurological or psychological symptoms to be immediately told to improve their diet, manage their stress, and continue to exercise. I want them to know that these changes will improve their disease course and health outcomes.
Changing The Standard Of CareThe Power of Hormonal Harmony: Why Maintaining Ideal Testosterone Levels Matters for Everyone

Exploring the Lifelong Advantages of Maintaining Healthy Testosterone Levels in Both Sexes
The Power of Hormonal Harmony: Why Maintaining Ideal Testosterone Levels Matters for EveryoneHistamine Intolerance and Mast Cell Activation

Some people are troubled by histamine intolerance. Histamine is produced and released by immune cells (mast cells and basophils).
Histamine Intolerance and Mast Cell ActivationHow to Make a Delicious Smoothie on the Wahls Protocol®

I started the Wahls Protocol® the first summer I was diagnosed with MS. The number of vegetables I now needed to consume in a day was intimidating to say the least. I took what little energy I had and threw every healthy food I could find into a blender. My smoothies looked like mud and tasted gross.
How to Make a Delicious Smoothie on the Wahls Protocol®Cortisol Demystified: Your Guide to Understanding the Body's Stress Regulator

When faced with a threat to our safety, our adrenal glands secrete cortisol, and the sympathetic nervous system releases epinephrine and norepinephrine. This causes our senses to heighten and makes us temporarily faster and stronger so we can flee the threat or defeat the thing threatening us. However, chronic elevation of these same hormones and neurotransmitters can cause health problems, diminishing sleep duration and quality and increasing the risk of insulin resistance, metabolic syndrome, and/or diabetes. It also puts us at higher risk for chronic fatigue, anxiety, and depression.
Cortisol Demystified: Your Guide to Understanding the Body's Stress RegulatorNeufit Helping MS Patients
Many people living with multiple sclerosis (or other neuroimmune conditions) are plagued with problems due to <strong>spasticity,</strong> <strong>pain,</strong> and <strong>cognitive issues</strong>. These are often the most common problem areas for patients.
Neufit Helping MS PatientsThe Strategies I Use for Getting Great Sleep

Sleep has always been difficult for me. For years it was difficult to fall asleep and stay asleep. Often I would wake up at 2 in the morning, unable to fall back asleep again. Earlier in my life, I was fine with sleeping only 4 or 5 hours at night. I was ambitious. I had a lot to do. I thought that sleeping was a waste of my time. I did that in college, medical school, during my residency, and when I began working as a physician. When I had Zach and Zebby, I thought it was an advantage that I slept so little. Now I know better.
The Strategies I Use for Getting Great SleepWhy Your B Vitamins Should Be Activated

Do you have a family history of neurological, psychiatric, or cardiovascular disease? I do–I have several uncles who developed angina in their 40s, aunts and uncles with neuroimmune problems affecting their peripheral nerves, and relatives with severe mood disorders. All these diagnoses in my family mean it’s likely I have genetic variants that affect how my body metabolizes B vitamins.
Why Your B Vitamins Should Be ActivatedHow To Trigger Healing With This Natural Remedy

Your Parasympathetic Nervous System affects EVERY aspect of your well-being! Digestion, detoxification, and immune functions are only turned on when your parasympathetic nervous system is activated.
How To Trigger Healing With This Natural RemedyCould Pomegranate Polyphenols Hold the Key to Longevity?

Having healthy strong mitochondria is necessary to have a healthy, strong body. It’s our mitochondria that generate the ATP through cells we use to drive the energy of life, the chemistry of life. And as we age, our mitochondria become less vigorous, and less vital. We know there are some ways to youthen your mitochondria. And this includes fasting, high-intensity interval training, and strength training—And there’s another compound Urolithin A.
Could Pomegranate Polyphenols Hold the Key to Longevity?How To Make Sleep A Priority

Sleep has been difficult for me most of my life. It is hard for me to fall asleep and harder to stay asleep.
How To Make Sleep A PriorityDiet— How Times Are Changing

The world is changing. Neurology and MS care are changing. It’s been a long journey to this point, and not an easy one. Let me tell you how we got here.
Diet— How Times Are ChangingDo you need activated b vitamins or an MTHFR Supplement?

Fatigue is one of top reasons people with multiple sclerosis (MS) leave employment. Cognitive decline is the next most common reason. I had years of relentlessly worsening fatigue. My neurologist gave me Provigil to treat the fatigue, which provided a slight improvement. I was still exhausted by 10 in the morning, but I definitely was more exhausted without it.
Do you need activated b vitamins or an MTHFR Supplement?Why you should shift your focus to your metabolic health

I have a family history of illness. My grandparents had diabetes. My father was severely obese, and on my mother’s side, I have multiple aunts and uncles with heart disease. Even though I am quite lean, I have risk factors for metabolic syndrome, including very low HDL cholesterol and higher triglycerides.
Why you should shift your focus to your metabolic healthIncreased blood clotting, heart disease risk…and eggs?

I have seen an uptick in inquiries surrounding blot clotting, cardiovascular health, and eggs as these are current topics of interest and have surfaced in a number of articles—both research-based and sensationalized. I want to address a Cleveland Clinic study from 2017 specifically.
Increased blood clotting, heart disease risk…and eggs?Mitigating The Risks Of Gluten Contamination

Mitigating The Risks Of Gluten Contamination People with Celiac disease follow a lifelong gluten-free diet to manage their condition. I too follow a strict gluten-free diet. When I travel, I am always concerned about being exposed to gluten–20-40% of restaurant foods that are labeled gluten-free and 20% of grocery items that are labeled gluten-free actually have detectable gluten in them.1,2
Mitigating The Risks Of Gluten ContaminationDr. Terry Wahls, Principal Investigator for the study “Efficacy of Diet on Quality of Life for Individuals Diagnosed with Relapsing-Remitting Multiple Sclerosis”

We are recruiting for a new study that is being conducted at the University of Iowa! You are invited to participate in a research study to evaluate the effects of three diets — <b>Modified Paleolithic Elimination diet</b>, <b>Time Restricted Olive Oil-based Ketogenic diet</b>, and <b>your usual diet</b> with the addition of educational materials. Participants in the usual diet group will receive educational information and determine if they would like to make any changes based on the recommendations provided. We will look at the effects of diet on quality of life, including motor and vision function, fatigue, mood, and disease activity. This will be assessed by online surveys, study participant tasks, and brain imaging.
Dr. Terry Wahls, Principal Investigator for the study “Efficacy of Diet on Quality of Life for Individuals Diagnosed with Relapsing-Remitting Multiple Sclerosis”How To Create A Personalized Wellness Center In Your Home

When the world locked down in 2020, an interesting shift in fitness and self-care took place. We realized that we can turn our homes into personalized wellness centers! Lifepro Fitness has been leading the charge in helping wellness-conscious people find affordable solutions to furnishing a comfortable, customized home-base for self-care!
How To Create A Personalized Wellness Center In Your HomeRocking Your Mitochondria

If you have multiple sclerosis or another autoimmune condition with neurological or psychological symptoms, you need to resuscitate your mitochondria. Mitochondria generate adenosine triphosphate (ATP), which are used by cells to drive the chemistry of life. There is increased recognition that brain cells, including neurons, astrocytes, and microglia, have very high energy needs and need lots of ATP, as do retinal cells and heart cells. If mitochondria are inefficient, cells begin to function inefficiently.
Rocking Your MitochondriaBrain Support

When I was younger, I ran and skied marathons. When I had kids, I transitioned to biking and skiing with my family. When she was little, I pulled Zebby in a sled behind me. When she was a bit older, she held a little wooden bar connected to a harness that I wore, like she was water skiing behind me. We all loved to ski, bike, and hike in the woods.
Brain SupportConquer cold and flu season
As we age the effectiveness of our immune cells declines and it takes a smaller dose of the pathogen to infect us. Over the age of 40, our immune cells begin being less effective and are much less effective over the age of 60. Having more medical problems also increases the risk of immune cell decline.
Conquer cold and flu seasonUse electrical stimulation to regain lost muscle function with Neufit

The unique properties of Neufit’s direct current stimulation device are making a dramatic difference in the lives of MS (multiple sclerosis) patients or patients who have lost function because of other neurological injuries or neurodegenerative diseases.
Use electrical stimulation to regain lost muscle function with NeufitIs Candida Taking Over Your Gut?
Increasingly scientists recognize the importance of our microbiome to health. The microbiome is a unique fingerprint—each individual has a slightly different microbiome that is stable and unique to them and influenced by major events in their early life. By the time we are three years old, our microbiome community has established itself. Unfortunately, I, like many with autoimmune disease, had a sub-optimal start to my microbiome, which faced several challenges that reduced its quality.
Is Candida Taking Over Your Gut?Do you include this essential nutrient when fueling your mitochondria?

Most people with neurological, psychological, cardiac, or ocular problems will benefit from a tune-up of their mitochondria.
Do you include this essential nutrient when fueling your mitochondria?Support detoxification, neurological function, and immune function

Sulfur is an important part of a health-promoting diet, which is why I stress cabbage and onion family vegetables. The body needs sulfur to manufacture glutathione, which is the master antioxidant in our cells. The body also needs sulfur to manufacture L-cysteine, an amino acid. Amino acids are the building blocks for structural and functional proteins and peptides (very short amino acid sequences) that are essential to human health. There are 20 essential amino acids and 10 conditionally essential amino acids. Essential means that we cannot make that particular amino acid. Conditionally essential means that if we have all the ingredients needed to make that amino acid, we can. L-Cysteine is a conditional amino acid, meaning that our body can make L-cysteine if there is enough sulfur in the diet to do so.
Support detoxification, neurological function, and immune functionAre you making this common vitamin D mistake?

Many clinicians and patients now know that vitamin D plays an important role in immune health, bone health and brain health.
Are you making this common vitamin D mistake?Managing the Emotions of MS

Enjoy this guest post from Wahls Health Practitioner, Alene Brennan from lesspharmmoretable.com What emotions ran through you first when you heard the words, “You have MS?” Fear… anger… relief… anxiety… defeat… all of the above? It’s been six years since I heard those words from my neurologist, and I still experience all the emotions. I […]
Managing the Emotions of MSDrivers of Mitochondrial Strain And What You Can Do About It
Fatigue is one of the most common problems I see in my clinics and studies. Many of those with autoimmune diseases struggle with it every day, but even people who don’t suffer from a chronic disease often complain of fatigue, relying on caffeine to get them through the afternoon. What people don’t often realize is that fatigue may be related to more than sleep deprivation. In my experience, fatigue is often a symptom of depleted and starved mitochondria, and the reason for depleted and starved mitochondria is frequently an insufficiently nutrient-dense diet, exacerbated by the nutrient-depleting effects of medication.
Drivers of Mitochondrial Strain And What You Can Do About ItHow to fix your bleeding gums

Unless you have actually cut your gums, bleeding is a sign of infection. Your gums should never bleed. Think about your fingernails. If you were scrubbing your nails with a scrub brush, it wouldn’t be normal for them to bleed, would it?
How to fix your bleeding gumsNutrients required for effective immune system function
It has been a few months since I wrote to you about the coronavirus situation and I wanted to send an encouraging update on my thoughts and findings.
Nutrients required for effective immune system functionWhy I Use A Continuous Glucose Monitor (CGM) To Manage My Multiple Sclerosis

I do not have diabetes or pre-diabetes, but I have used a continuous glucose monitor for months to learn about my metabolic health. I care a lot about my metabolic health because I have secondary progressive multiple sclerosis and have experienced depression, and poor metabolic health worsens autoimmunity and mental illness.
Why I Use A Continuous Glucose Monitor (CGM) To Manage My Multiple SclerosisThis Army Apache Pilot Reversed His Hashimoto’s And Reclaimed His Career With These Nutrient Dense Soups

I am thrilled to tell you about this amazing company I have connected with: <a href="https://captainsoup.com/" target="_blank">Captain Soup</a>. This medical diet-focused company has created delicious grab-and-go meals made from the highest quality grass-fed and organic ingredients available.
This Army Apache Pilot Reversed His Hashimoto’s And Reclaimed His Career With These Nutrient Dense SoupsAre You Protecting Your Cell Membranes? An Overlooked Wellness Strategy

Could the complex diseases of today be healed by addressing the fats and oils of the cell membrane?
Are You Protecting Your Cell Membranes? An Overlooked Wellness StrategySauna for more than detox

A number of factors in modern living have created a really toxic tidal wave that is nearly impossible for us to escape. There is good news though—we can trick our bodies into thinking they are living in the ancestral environment that helped us evolve into the humans we are today.
Sauna for more than detoxRepair damage that occurs to the central nervous system
Most of us want to stay healthy as we age and be able to repair any damage that occurs to our central nervous system, that is our brain and spinal cord. Microglia and astrocytes play a big role in that process1,2. They provide structure and support for the neurons, the brain cells that receive signals from our sensory organs and send signals to our muscles. Astrocytes are also important for the blood-brain barrier, providing nutrients and oxygen to our neurons. Microglia are the immune cells of the central nervous system. Depending on the microenvironment, your microglia and astrocytes may be healing your brain or creating more damage, which can lead to more disease and rapid aging.
Repair damage that occurs to the central nervous systemFive Steps For Increasing Longevity

I plan to live a rich and full life until I’m 120 years old, gardening and playing soccer and euchre with my family. The most critical actions we can take now to keep our bodies and brains healthy for decades to come are […]
Five Steps For Increasing LongevityDEFYING ALL ODDS: Un DOCUMENTAIRE SUR LE PARCOURS DE RÉTABLISSMENT DU DR WAHLS
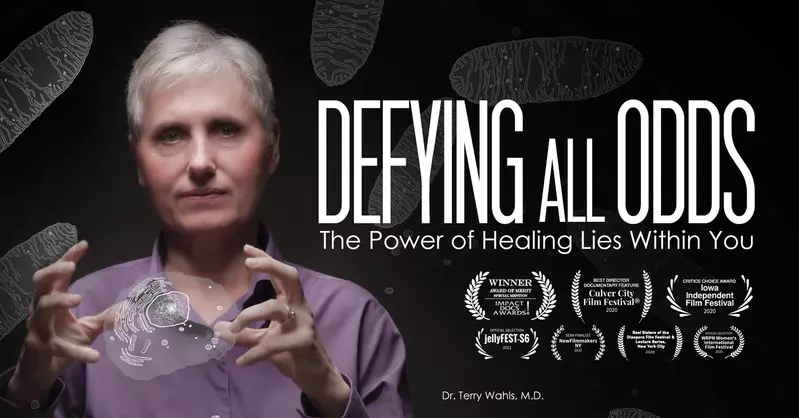
On me demande souvent comment j’en suis venu à faire un documentaire sur le parcours de rétablissement de la sclérose en plaques du Dr Wahls.
DEFYING ALL ODDS: Un DOCUMENTAIRE SUR LE PARCOURS DE RÉTABLISSMENT DU DR WAHLSThe gut-brain immune connection is now recognized to be a factor in neurological issues

Increasingly people are aware that the health of their microbiome determines how well their cells run the chemistry of life. The gut-brain-immune connection is now recognized by more primary care physicians and specialists as well as patients as an important factor in restoring health for those with neurological1,2, psychiatric3, and/or autoimmune conditions4,5. People often ask me if they need to eat fiber and fermented food to reset their microbiome, or if they can just take supplements instead and keep eating what they want.
The gut-brain immune connection is now recognized to be a factor in neurological issuesNew Wahls Research: Swank Diet Vs Wahls Elimination Diet
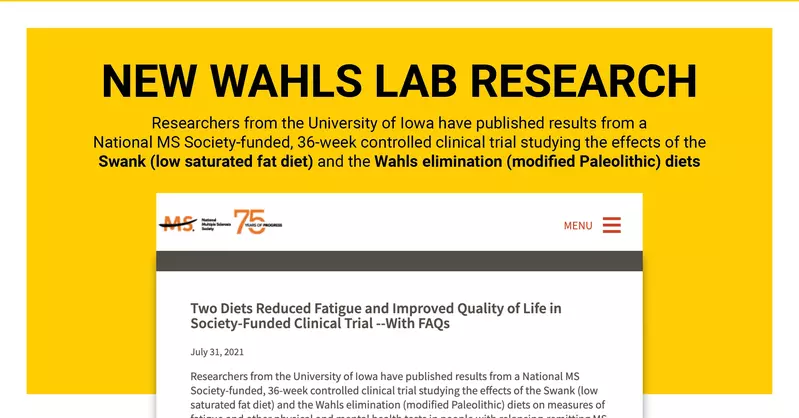
We finally did it! We have published the results from our study of the Swank diet versus the Wahls diet in <em><a href="https://journals.sagepub.com/doi/10.1177/20552173211035399" target="_blank">Multiple Sclerosis Journal – Experimental, Translational and Clinical</a>,</em> an international, peer-reviewed publication. This is a tremendously exciting moment for our research team and for all multiple sclerosis patients around the globe, one that has been more than a decade in the making.
New Wahls Research: Swank Diet Vs Wahls Elimination DietDo you have an autoimmune prodrome? My top 5 tips to stop your body from attacking itself.
Do you have worsening fatigue, headache, brain fog, problems with mood and concentration, physical pain, or unsteadiness, but your medical team can’t find anything wrong with you? Maybe you have some mild elevation of autoantibodies, but not enough for doctors to come up with a diagnosis. Your doctors may be reassuring, but you know your immune cells should not be attacking and damaging parts of your body. Or maybe you have migraines, chronic pain, unexplained fatigue or other unexplained symptoms.
Do you have an autoimmune prodrome? My top 5 tips to stop your body from attacking itself.Defying All Odds: a documentary about Dr. Wahls’ recovery journey
I am often asked how I came about making a documentary about Dr. Wahls’ recovery journey from MS. Today, I would like to share this story with you…
Defying All Odds: a documentary about Dr. Wahls’ recovery journeyA2 milk from goats, sheep and other animals: Friend or foe?

I am often asked if A2 milk, which is milk from goats or sheep, is a good alternative to A1 milk, which is from Holsteins, the black and white dairy cows that predominate American dairy production.
A2 milk from goats, sheep and other animals: Friend or foe?Fermented foods and histamine intolerance
What do you do when foods you consider “healing foods” give you symptoms like headache, hives, or stuffy sinuses? While fermented foods like sauerkraut and kimchi are highly nutritious they may be the source of these symptoms due to an intolerance to histamine.
Fermented foods and histamine intoleranceThe problem with mushroom products on the market

<em>I do want to let you know that the team at <a href="https://terrywahls.com/" target="_blank">terrywahls.com</a> does receive a small affiliate commission for any product ordered through Paleovalley. This is part of how we are able to produce so many informational resources at no cost to you. If you’re not comfortable with an affiliate link—no worries, I hope that you do find the information shared to be beneficial!</em>
The problem with mushroom products on the marketMy top tips to increase strength and improve rehab

What’s one of the most powerful things that you can do to increase strength and improve your rehabilitation efforts?
My top tips to increase strength and improve rehabThe Benefits Of Light & Sauna Therapy For Autoimmune And Chronic Conditions

This interview with Wahls Protocol® Virtual Seminar Sponsor, <a href="https://sauna.space/?rfsn=3337837.d81318" target="_blank">SaunaSpace</a> explains how you may be able to overcome heat intolerance and expand your healing capacity with the incandesce of a natural thermal light spectrum of red, near-infrared and thermal infrared light wavelengths.
The Benefits Of Light & Sauna Therapy For Autoimmune And Chronic ConditionsAsk the Experts: Simple Wellness Strategies To Mitigate Infection Risks

The coronavirus. The influenza virus. We anticipate that the rate of infection for both of these viruses will increase over the winter. What can you do to lower the risk of acquiring both influenza and the coronavirus? What can you do to make it more likely, if you do acquire either of those infections, that you’ll have a relatively mild course and that you will be less likely to need the hospital and less likely to develop the long-hauler syndrome?
Ask the Experts: Simple Wellness Strategies To Mitigate Infection RisksMy Vision To Create An Epidemic Of Health

My dream of creating an epidemic of health and helping address chronic inflammation and chronic disease is more critical than ever.
My Vision To Create An Epidemic Of HealthCell Membrane Medicine
![bodybio-social2[1]](/media/667ba78e69bde3f938b8ede3/large.webp)
A turning point in my recovery happened when I dove deep into understanding how my cells run the chemistry of life. It wasn’t until then that I thought deeply about how lifestyle factors (diet, environment, genetics, etc.) were impacting the health of my cells.
Cell Membrane MedicineThe Role of E Stim in Rehab and Recovery: Neurodegenerative Diseases or Neurological Injuries
The electrical stimulation of muscles was a large part of Dr. Terry Wahls’ recovery after years of steady decline with Multiple Sclerosis. Today she uses <a href="https://www.neu.fit/" target="_blank">Neufit’s</a> Neubie device as a vigorous part of her daily workout and rehab program.
The Role of E Stim in Rehab and Recovery: Neurodegenerative Diseases or Neurological InjuriesUPDATED: CORONAVIRUS—What You Can Do To Reduce Your Risk Of Complications

Information about COVID-19 continues to evolve rapidly. In this article, I am adding a brief discussion about cytokine storm, citations, and additional strategies to consider.
UPDATED: CORONAVIRUS—What You Can Do To Reduce Your Risk Of ComplicationsA Nutritionist's Approach to Functional Medicine

In this interview, Dr. Wahls and Natasha Azrak discuss how to get the most benefit from a functional medicine intervention without expensive testing or supplements. Natasha Azrak is the first and only nutritionist certified by the Institute for Functional Medicine in Canada and the only French-speaking in the world. She is also a Wahls Protocol® Health Professional.
A Nutritionist's Approach to Functional MedicineWahls Protocol Health Practitioner Spotlight: Andrea Sprague, Chef, F-NTP

Andrea helps clients learn to love food again after food allergies or a healing crisis causes them to radically change their diets. She became a chef because of her own food allergies and discovered not just her love of cooking, but a new way to feed herself that completely eliminated the symptoms that had plagued her for years. Through her own health journey, she discovered the immense healing power food can have and dedicated her life to helping others heal in the same way.
Wahls Protocol Health Practitioner Spotlight: Andrea Sprague, Chef, F-NTPMS Management and My Medicinal Mushroom Trio
I was diagnosed with MS over 20 years ago. At the time, I was completely overwhelmed by the MRI that showed lesions in my brain, by the loss of my eyesight, and by how quickly I went downhill. I was scared, and I followed my neurologist’s orders. Back then, alternative medicine was, well, alternative. My doctor never asked me about my diet or my lifestyle. He simply gave me drugs – and then he gave me more drugs to counteract the side effects. I was on medication to combat muscle spasms and fatigue, and I started daily injections of Copaxone. But I kept getting worse.
MS Management and My Medicinal Mushroom TrioThree Steps To Avoid Losing Your Medical License Over Anonymous Complaints
If you are a physician, physician assistant, advanced practice registered nurse, registered dietitian, therapist, or chiropractor, it is critical to protect your medical or health-related license.
Three Steps To Avoid Losing Your Medical License Over Anonymous ComplaintsLiving with Lyme Disease, Multiple Sclerosis, and Mold with Dr. Terry Wahls & Dr. Darin Ingels
Dr. Ingels is a respected leader in natural medicine with numerous publications, international lectures and 30 years of experience in the healthcare field. He received his Bachelor of Science degree in medical technology from Purdue University and his Doctorate of Naturopathic Medicine from Bastyr University in Seattle, Washington. Dr. Ingels completed his residency at the Bastyr Center for Natural Health.
Living with Lyme Disease, Multiple Sclerosis, and Mold with Dr. Terry Wahls & Dr. Darin IngelsWahls Peer-Reviewed Publications in the High-Impact Nutrition Journal Nutrients

I am one of the few health and wellness authors who also does research on the impact of dietary interventions.
Wahls Peer-Reviewed Publications in the High-Impact Nutrition Journal NutrientsWahls Peer-Reviewed Research: Neuromuscular electrical stimulation and dietary interventions to reduce oxidative stress in a secondary progressive multiple sclerosis patient leads to marked gains in function: a case report

Reese D, Shivapour ET, Wahls TL, Dudley-Javoroski SD, Shields R. Cases Journal. 2009;2:7601. PMID:19918474 <a href="https://pubmed.ncbi.nlm.nih.gov/19918474/" target="_blank">Read the paper, click here</a>
Wahls Peer-Reviewed Research: Neuromuscular electrical stimulation and dietary interventions to reduce oxidative stress in a secondary progressive multiple sclerosis patient leads to marked gains in function: a case reportWahls Peer-Reviewed Research: Nutrient Composition Comparison between the Low Saturated Fat Swank Diet for Multiple Sclerosis and Healthy U.S.-Style Eating Pattern

Chenard C, Rubenstein L, Snetselaar L, **Wahls T**. <a href="https://pubmed.ncbi.nlm.nih.gov/30871265/" target="_blank">Nutrients.</a> 2019 Mar 13;11(3). pii: E616. doi: 10.3390/nu11030616. PMID: 30871265 <a href="https://pubmed.ncbi.nlm.nih.gov/30871265/" target="_blank">Read the paper, click here</a>
Wahls Peer-Reviewed Research: Nutrient Composition Comparison between the Low Saturated Fat Swank Diet for Multiple Sclerosis and Healthy U.S.-Style Eating PatternWahls Peer-Reviewed Research: Randomized control trial evaluation of a modified Paleolithic dietary intervention in the treatment of relapsing-remitting multiple sclerosis: a pilot study

Irish A, Erickson CE, Wahls TL, Snetselaar L, Darling WR. Degenerative Neurological and Neuromuscular Diseases. 2017 September 8;7:1-18. doi: <a href="https://www.dovepress.com/randomized-control-trial-evaluation-of-a-modified-paleolithic-dietary--peer-reviewed-fulltext-article-DNND" target="_blank">https://www.dovepress.com/randomized-control-trial-evaluation-of-a-modified-paleolithic-dietary--peer-reviewed-fulltext-article-DNND</a>. <a href="https://pubmed.ncbi.nlm.nih.gov/30050374/" target="_blank">Read the paper, click here</a>
Wahls Peer-Reviewed Research: Randomized control trial evaluation of a modified Paleolithic dietary intervention in the treatment of relapsing-remitting multiple sclerosis: a pilot studyWahls Peer-Reviewed Research: Rehabilitation with neuromuscular electrical stimulation leads to functional gains in ambulation in patients with secondary progressive and primary progressive multiple sclerosis: a case series report

Wahls TL, Reese D, Kaplan D, Darling WG. Journal of Alternative and Complementary Medicine (New York, N.Y.). 2010 December;16(12):1343-9. PMID:21138391 <a href="https://pubmed.ncbi.nlm.nih.gov/30050380/" target="_blank">Read the paper, click here</a>
Wahls Peer-Reviewed Research: Rehabilitation with neuromuscular electrical stimulation leads to functional gains in ambulation in patients with secondary progressive and primary progressive multiple sclerosis: a case series reportWahls Peer-Reviewed Research: The Seventy Percent Solution

<a href="https://pubmed.ncbi.nlm.nih.gov/21253878/" target="_blank">Read the paper, click here</a>
Wahls Peer-Reviewed Research: The Seventy Percent SolutionWahls Peer-Reviewed Research: Telling The World

<a href="https://www.ncbi.nlm.nih.gov/pubmed/18591640" target="_blank">Read the paper, click here</a>
Wahls Peer-Reviewed Research: Telling The WorldWahls Peer-Reviewed Research: A multimodal intervention for patients with secondary progressive multiple sclerosis: feasibility and effect on fatigue

Bisht B, Darling WG, Grossmann RE, Shivapour ET, Lutgendorf SK, Snetselaar LG, Hall MJ, Zimmerman MB, Wahls TL. J Altern Complement Med. 2014 May 1;20(5):347-55. PMID:24476345. doi: 10.1089/act.2014.20606.
Wahls Peer-Reviewed Research: A multimodal intervention for patients with secondary progressive multiple sclerosis: feasibility and effect on fatigueWahls Peer-Reviewed Research: A Multimodal, Nonpharmacologic Intervention Improves Mood and Cognitive Function in People with Multiple Sclerosis

Lee JE, Bisht B, Hall MJ, Rubenstein LM, Louison R, Klein DT, Wahls TL. Journal of the American College of Nutrition. 2017 April 10:1-19. PMID:28394724. doi: 10.1080/07315724.2016.1255160. <a href="https://pubmed.ncbi.nlm.nih.gov/28394724/" target="_blank">Read the paper, click here</a>
Wahls Peer-Reviewed Research: A Multimodal, Nonpharmacologic Intervention Improves Mood and Cognitive Function in People with Multiple SclerosisWahls Peer-Reviewed Research: Assessment of Dietary Adequacy for Important Brain Micronutrients in Patients Presenting to a Traumatic Brain Injury Clinic For Evaluation

Wahls T, Rubenstein L, Hall M, Snetselaar L. Nutr Neurosci. 2014 November 1;17(6):252-9. PMID:24074905. doi: 10.1179/1476830513Y.0000000088. <a href="https://pubmed.ncbi.nlm.nih.gov/24074905/" target="_blank">Read the paper, click here</a>
Wahls Peer-Reviewed Research: Assessment of Dietary Adequacy for Important Brain Micronutrients in Patients Presenting to a Traumatic Brain Injury Clinic For EvaluationWahls Peer-Reviewed Research: Dietary approaches to treat MS-related fatigue: comparing the modified Paleolithic (Wahls Elimination) and low saturated fat (Swank) diets on perceived fatigue in persons with relapsing-remitting multiple sclerosis: study protocol for a randomized controlled trial

Wahls T, Scott MO, Alshare Z, Rubenstein L, Darling W, Carr L, Smith K, Chenard CA, LaRocca N, Snetselaar L. Trials. 2018 June 4;19(1):309. PMID:29866196. doi: 10.1186/s13063-018-2680-x.
Wahls Peer-Reviewed Research: Dietary approaches to treat MS-related fatigue: comparing the modified Paleolithic (Wahls Elimination) and low saturated fat (Swank) diets on perceived fatigue in persons with relapsing-remitting multiple sclerosis: study protocol for a randomized controlled trialWahls Peer-Reviewed Research: Effects of a multimodal intervention on gait and balance of subjects with progressive multiple sclerosis: a prospective longitudinal pilot study

Bisht B, Darling WG, White EC, White KA, Shivapour ET, Zimmerman MG, Wahls TL. Journal of Degenerative Neurological and Neuromuscular Disease. 2017 June 26;7:79-93. doi: <a href="https://www.dovepress.com/effects-of-a-multimodal-intervention-on-gait-and-balance-of-subjects-w-peer-reviewed-fulltext-article-DNND" target="_blank" >https://www.dovepress.com/effects-of-a-multimodal-intervention-on-gait-and-balance-of-subjects-w-peer-reviewed-fulltext-article-DNND</a>. <a href="https://pubmed.ncbi.nlm.nih.gov/30050380/" target="_blank" >Read the paper, click here</a>
Wahls Peer-Reviewed Research: Effects of a multimodal intervention on gait and balance of subjects with progressive multiple sclerosis: a prospective longitudinal pilot studyWahls' Research Papers: Lipid Profile is Associated with Decreased Fatigue in Individuals with Progressive Multiple Sclerosis Following a Modified Paleolithic Diet-Based Intervention: Results from a Pilot Study, PLoS One
Fellows K, <strong>Wahls T</strong>, Brown R, Rubenstein R, Chenard C, Snetselaar L, Weinstock-Guttman B, Ramanthan M. 2019 Jun 18;14(6):e0218075. doi: 10.1371/journal.pone.0218075. eCollection 2019
Wahls' Research Papers: Lipid Profile is Associated with Decreased Fatigue in Individuals with Progressive Multiple Sclerosis Following a Modified Paleolithic Diet-Based Intervention: Results from a Pilot Study, PLoS OneWahls Peer-Reviewed Research: Multimodal intervention improves fatigue and quality of life of subjects with progressive multiple sclerosis: a pilot study

Bisht B, Darling W, Grossman R, Shivapour E, Lutgendorf S, Snetselaar L, Hall M, Zimmerman M, Wahls T. Journal of Degenerative Neurological and Neuromuscular Disease. 2015 February 27;2015:5:19-35. doi: <a href="https://www.dovepress.com/multimodal-intervention-improves-fatigue-and-quality-of-life-in-subjec-peer-reviewed-fulltext-article-DNND" target="_blank">https://www.dovepress.com/multimodal-intervention-improves-fatigue-and-quality-of-life-in-subjec-peer-reviewed-fulltext-article-DNND</a>. <a href="https://www.dovepress.com/multimodal-intervention-improves-fatigue-and-quality-of-life-in-subjec-peer-reviewed-fulltext-article-DNND" target="_blank">Read the paper, click here</a>
Wahls Peer-Reviewed Research: Multimodal intervention improves fatigue and quality of life of subjects with progressive multiple sclerosis: a pilot studyWahls Peer-Reviewed Research: Nutrient Composition Comparison between a Modified Paleolithic Diet for Multiple Sclerosis and the Recommended Healthy U.S.-Style Eating Pattern

Chenard C, Rubenstein L, Snetselaar L, **Wahls T**. , Nutrients. 2019 March 1;11(3):537. PMID:30832289. doi: 10.3390/nu11030537. <a href="https://pubmed.ncbi.nlm.nih.gov/30832289/" target="_blank">Read the paper, click here</a>
Wahls Peer-Reviewed Research: Nutrient Composition Comparison between a Modified Paleolithic Diet for Multiple Sclerosis and the Recommended Healthy U.S.-Style Eating PatternWahls Peer Reviewed Reserach: Review of Two Popular Eating Plans within the Multiple Sclerosis Community: Low Saturated Fat and Modified Paleolithic

<strong>Wahls T</strong>, Chenard C, Snetselaar L. ., Nutrients. 2019 February 7;11(2):E352. PMID:30736445. doi: 10.3390/nu11020352. <a href="https://www.ncbi.nlm.nih.gov/pubmed/30736445" target="_blank">Read the paper, click here</a>
Wahls Peer Reviewed Reserach: Review of Two Popular Eating Plans within the Multiple Sclerosis Community: Low Saturated Fat and Modified PaleolithicA review of research studies and clinical cases in Japan suggests role of gut environment in development of multiple sclerosis
Gut is the largest immune organ with vast number and variety of immune cells residing in it. It is thought that gut-residing immune cells move to central nervous system (brain and spinal cord) and can affect neurological conditions like multiple sclerosis (MS). In a recent review published in the journal “Neurochemistry International” (published May 2019, <a href="https://www.ncbi.nlm.nih.gov/pubmed/31152766" target="_blank">https://www.ncbi.nlm.nih.gov/pubmed/31152766</a>, authors took into consideration various type of studies including epidemiological, clinical cases and microbiome studies and pointed out the role of environmental factors especially dietary changes in development of MS.
A review of research studies and clinical cases in Japan suggests role of gut environment in development of multiple sclerosisResearch Update: The link between our gut microbiome, inflammation in the brain and speed of brain shrinkage
It is so great to see another <a href="https://pubmed.ncbi.nlm.nih.gov/31242699/" target="_blank">paper</a> talking about the link between our gut microbiome and the level of inflammation in the brain and speed of brain shrinkage. The evidence grows that the microbes in our gut speak directly to our immune cells and our brain cells. Even more exciting is the evidence that our microbes influence our ability to repair our myelin. And our clinical partners are recognizing that diet matters because diet influences the microbiome.
Research Update: The link between our gut microbiome, inflammation in the brain and speed of brain shrinkageDefying All Odds
The team at Defying All Odds film are very excited to be at the end stages of completing this project and can’t wait to see it out on the big screen!
Defying All OddsPhosphatidylcholine for detoxification and cellular health
<a href="http://bodybio.com/discount/WAHLS-P" target="_blank">BodyBio</a> is a nutritional supplement company that is relentlessly focused on the pursuit of health at the cellular level. BodyBio products stand out from many of the vitamins and supplements on the market because our products were originally created for those with complex disorders over 25 years ago. The founders of BodyBio are leading researchers in the field of complex metabolic disorders, fatty acid analysis, neurodegenerative diseases
Phosphatidylcholine for detoxification and cellular healthResearch Alert: Effect of Exercising Using Whole Body Vibration in Patients with Neurological Disorders
In the <a href="https://pubmed.ncbi.nlm.nih.gov/31246611/" target="_blank">paper linked here</a>, there is a discussion of the effect of exercising using whole body vibration.
Research Alert: Effect of Exercising Using Whole Body Vibration in Patients with Neurological DisordersE-Stim for MS
Follow me over the next few months as I work with Neufit’s team to build strength and optimize my workouts. Learn more at neu.fit/wahlsprotocol
E-Stim for MSNear-Infrared Light and Heat: Nature’s Most Powerful Healing Detox Solution
Medical experts will often paint a hopeless picture, especially when it comes to natural alternatives, for MS patients and those suffering from co-infections such as Lyme disease. Many feel abandoned and left in the dark. There is, however, a ray of hope beginning to emerge. Because experts on chronic infections and neuropathic disease have found […]
Near-Infrared Light and Heat: Nature’s Most Powerful Healing Detox SolutionNeuroinflammation Spectrum

They might have multiple sclerosis, clinically isolated syndrome, or optic neuritis, or perhaps are affected by other serious autoimmune diseases, like Celiac, Systemic Lupus, Rheumatoid Arthritis, or Inflammatory Bowel Disease. Symptoms may include fatigue, problems with balance and coordination, numbness, and muscular weakness. These symptoms can go on for years, sometimes decades, slowly worsening and wearing us down.
Neuroinflammation SpectrumStarting the Wahls Protocol® Without the Overwhelm – From a Wahls Warrior and Health Coach
It is Multiple Sclerosis Awareness Month, and I am featuring a guest post from a Wahls Warrior™ and Wahls Certified Health Coach, Alene Brennan:
Starting the Wahls Protocol® Without the Overwhelm – From a Wahls Warrior and Health CoachHere’s My Secret Needle Mover for Fat Loss By Dr. Anna Cabeca
She was sticking with a well-designed ketogenic diet that incorporated plenty of veggies and other alkaline foods, exercising consistently, and following other lifestyle factors that I had recommended.
Here’s My Secret Needle Mover for Fat Loss By Dr. Anna CabecaWhy I am doing E Stim

E Stim was a large part of my recovery. To get stronger and optimize my daily workouts, I am working with the team at using their Neubie device. Follow me over the next few months to see how I use it in my daily routine.
Why I am doing E StimKetogenic Diets: How to Avoid Pitfalls and Maximize Benefits
Nutritional ketosis means that our mitochondria are burning fat instead of glucose (carbohydrates) or amino acids (protein) to generate energy (ATP). We do this when access to food is limited, as would occur during famine, drought, winter, or war. Diabetic ketoacidosis is a metabolic problem that occurs when the person has too little insulin and very high blood sugar. That is a critical health problem. Nutritional ketosis is a normal response to limited access to food when the body relies on its own fat stores.
Ketogenic Diets: How to Avoid Pitfalls and Maximize BenefitsBenefits of Exercise for Multiple Sclerosis (MS)

Movement as medicine. This blog post originally appeared at<a href="http://www.primalplay.com" title="" target="_blank">primalplay.com</a>and was reposted with permission from my good friend, movement coach and Wahls Certified Health Professional, Darryl Edwards. Source: <a href="https://www.primalplay.com/blog/benefits-of-physical-activity-for-multiple-sclerosis/" title="" target="_blank">The Benefits of Exercise for Multiple Sclerosis</a>
Benefits of Exercise for Multiple Sclerosis (MS)Learn more about Neufit Electrical Stimulation & Neubie

I get dozens of questions each week about using electrical stimulation therapy (e-stim). <a href="https://www.neu.fit" target="_blank">Neufit</a> was a sponsor at the 2018 seminar and founder Garrett Salpeter shares his experience using this refined technology in the field of physical rehabilitation and with people who have neurological and neurodegenerative issues. Try to make it to the end of the video to hear how seminar attendees responded to their Neufit sessions throughout the event weekend!
Learn more about Neufit Electrical Stimulation & NeubieNearinfared sauna detoxification

After my 3 week trip to Australia, I spent a considerable amount of time in the sauna after my long flights to detox from all of the environmental toxins I was exposed to during my 2o+ hours of travel — jet fuel fumes, radiation, plastics, etc.
Nearinfared sauna detoxificationA future of food, great teeth, and healthy guts
![lin-thumb[1]](/media/6679599a69bde3f938b8eaf5/original.webp)
Listen to the interview between Dr. Steven Lin and I about food, great teeth and healthy guts.
A future of food, great teeth, and healthy gutsAre Bleeding Gums the First Sign of Auto-Immunity?
![end-card-v2-lin[1]](/media/667a766c69bde3f938b8ebd0/large.webp)
As a dentist, I would often dread removing the last teeth from a person’s dentition. No one wants to lose any teeth, yet, I would see patients in their 30s and 40s with such severe periodontal disease, I would need to extract their last teeth.
Are Bleeding Gums the First Sign of Auto-Immunity?Red/Near-Infrared Light Therapy and Heat Therapy PLUS DETOX your body from stressful EMF

With the new year just a few weeks away, you can resolve to create better health for yourself in 2018. Along with a healthy diet, managing stress and reducing environmental toxin exposure–optimizing detoxification is a significant part of The Wahls Protocol®.
Red/Near-Infrared Light Therapy and Heat Therapy PLUS DETOX your body from stressful EMFThe Easiest, Most Effective Way to Harness Your Evolutionary Heritage to Re-Optimize Your Epigenetics Every Single Day

The ancestral human lived outdoors. Each day we experienced the natural full-spectrum light and heat of the Sun. Only recently have we shifted to spending our waking lives indoors, depriving our bodies of a vital nutrient and the forgotten cornerstone for achieving optimal health: full spectrum incandescent light and heat.
The Easiest, Most Effective Way to Harness Your Evolutionary Heritage to Re-Optimize Your Epigenetics Every Single DayGetting the Whole Family on Board or How I Conquered Our Dinner Table Problem

-by Heather Christo Both of my young daughters and I were all diagnosed with severe food allergies at about the same time. I have to admit, if it had only been me with the problem, I would have been tempted to sweep it under the carpet and try to minimize the impact on friends and […]
Getting the Whole Family on Board or How I Conquered Our Dinner Table Problem7 Ways to Optimize Cholesterol - by Dr. Hyman

“My doctor says my LDL cholesterol is really high and he’s concerned,” is a recent question I received from a reader. “Now you’re saying that I should <a href="https://drhyman.com/blogs/content/separating-fat-from-fiction-10-fat-facts-you-need-to-know/" target="_blank">eat more fat</a> , which should improve my cholesterol. I thought fat was the last thing I should be eating with high cholesterol.”
7 Ways to Optimize Cholesterol - by Dr. HymanAnnouncing The All New Wahls Protocol® Premium Menus And Recipes
This incredible program includes a year of access to menus, recipes, and shopping lists for your selected Diet plan (Wahls™, Wahls Paleo™, or Wahls Paleo Plus™) and weekly email notification with links to the menus, recipes, and shopping lists.
Announcing The All New Wahls Protocol® Premium Menus And RecipesSara Wahls – Inflammation Caused by Food Sensitivities

<strong>Who am I? I am Sara T. Wahls, a woman approaching 50, in a happy relationship celebrating 16 years this fall, who likes her job, and enjoys a variety of active hobbies. I am not a scientist, teacher, writer or nutritionist. But I do value helping others better address their health by sharing what I have learned. <a href="/blog/" >Here is my story</a>.</strong>
Sara Wahls – Inflammation Caused by Food SensitivitiesDr. Wahls and the Wahls Protocol® – Making me well

Dr. Terry Wahls and The Wahls Protocol® have made many people well. This song is dedicated to those that have been helped by the Wahls Protocol®. To learn more about Dr. Wahls, sign up for her email list, and order The Wahls Protocol® today.
Dr. Wahls and the Wahls Protocol® – Making me well“Could Your Diet Actually Be Fat-Deficient?” by Jimmy Moore

We’ve all grown up in a world where dietary fat is the enemy to our health. It’s “common knowledge” that to lose weight and to be healthy, you must reduce the amount of fat you are consuming in your diet leading people to make it their default plan a low-fat, low-calorie diet.
“Could Your Diet Actually Be Fat-Deficient?” by Jimmy MooreDr. Wahls’ Favorite Foods and Recipes

Dr. Terry Wahls reviews her favorite Foods and Recipes. She talks about what her daughter discovered as a favorite food as well. She also talks about some of the fresh foods she gets from her garden.
Dr. Wahls’ Favorite Foods and Recipes6 Tips For Loving Your Gut And Healing Digestive Problems Naturally – Dr. Sara Gottfried

It gives you that “gut reaction” when something isn’t quite right; it growls when you’re hungry; and a stomach upset is sometimes the first symptom of something amiss in your body. Indeed, <strong>your gut may be the most forthcoming part of your body</strong>, unable to mask the symptoms when something is wrong – and that’s a good thing.
6 Tips For Loving Your Gut And Healing Digestive Problems Naturally – Dr. Sara GottfriedDr. Terry Wahls’ Protocol That Reversed Multiple Sclerosis

Rhonda Patrick, PhD interviewed me in Austin Texas during the Paleo FX conference this year. The podcast is called <a href="https://www.patreon.com/posts/697928" target="_blank">Dr. Terry Wahls’ Protocol That Reversed Multiple Sclerosis</a>.
Dr. Terry Wahls’ Protocol That Reversed Multiple SclerosisDetox Summit Aug 4-11

<a href="https://dm177.infusionsoft.com/go/detoxreg/terrywahls/%20" target="_blank">Sign up</a> for the online Detox Summit starting August 4th. There are many experts on the topic, myself included. Register now to get access.
Detox Summit Aug 4-11Dr. Wahls on Fox 4 News

Dr. Wahls speaks on <a href="http://fox4kc.com/2014/04/28/doctor-confined-to-wheelchair-walks-again-by-changing-her-diet/">Fox 4 News</a> about her experiences with multiple sclerosis and the development of the Wahls Protocol®.
Dr. Wahls on Fox 4 NewsKansas City Live

On April 28th, I was on Kansas City Live. You can watch that here:Terry Wahls, M.D. discusses her new book ‘The Wahls Protocol®: How I Beat Progressive MS’.
Kansas City LiveDr. Wahls is at Paleo f(x)!

I am currently speaking at the Paleo f(x) conference this month. See my Paleo f(x) speaker portfolio. Find out what Paleo f(x) is all about here. Paleo f(x) is a marvelous opportunity for you to listen to various Paleo experts. Get the videos of Paleo f(x) or watch the conference virtually via live streaming video.
Dr. Wahls is at Paleo f(x)!Dr. Wahls’ interview with Examiner

Research is showing that there may be a link between mental health and the consumption of a ketogenic diet, giving hope to those who suffer from depression or bipolar disease. Ketogenic diets — which include high amounts of fat, adequate amounts of protein, and low amounts of carbohydrates — may also benefit those with other diseases, such as epilepsy, Parkinson’s disease, and multiple sclerosis.
Dr. Wahls’ interview with ExaminerCould Vegetarianism Increase Your Risk of Autoimmune Disease?

When I was a senior in high school, I read <i>Diet for a Small Planet</i> and became a vegetarian. Although I lived on a farm in rural Iowa, I decided that it was morally wrong to raise and kill animals for food and that a vegetarian diet was more environmentally sustainable.
Could Vegetarianism Increase Your Risk of Autoimmune Disease?Surviving and Thriving After a Multiple Sclerosis Diagnosis

<a href="https://www.iowapublicradio.org/show/river-to-river/2014-03-13/surviving-and-thriving-after-a-multiple-sclerosis-diagnosis" target="_blank">Iowa Public Radio interviews Dr. Wahls</a> about how she is surviving and thriving after her multiple sclerosis diagnosis. Dr. Wahls explains how she first noticed her symptoms in medical school, beginning with visual dimming, which became more severe over time. After multiple exams and misdiagnoses, she was told she had MS and was put on immune suppression drugs. Dr. Wahls talks about how she began reading research on autoimmune disease and found mitochondrial health to be a common thread in all brain disorders. In all cases, cell biochemistry was broken and mitochondria were sending “time to die” signals too early.
Surviving and Thriving After a Multiple Sclerosis DiagnosisCan Children Follow The Wahls Protocol®?

One question that many have asked me is whether children can follow The Wahls Protocol®, especially when the rest of the family is following it. Watch the video to hear my response.
Can Children Follow The Wahls Protocol®?Dr. Sara Gottfried

If you tried to access Dr. Gottfried’s offer before, you most likely received an error or notification that it was sold out. Dr. Gottfried has created a free gift package that includes the Hormone Toolkit and an extra gift as well all for free. The gifts expire on March 30th, so make sure to claim them in our latest newsletter email or contact Dr. Gottfried’s customer service.
Dr. Sara GottfriedDr. Wahls Interview with Five to Thrive

Dr. Wahls speaks with Five to Thrive co-host, Dr. Lise Alschuler. In this interview, Dr. Wahls shares her experience with multiple sclerosis and explains how MS is caused by inflammation of the central nervous system and oxidative stress on mitochondria. Other topics covered include food sensitivities, Dr. Wahls’ Paleo approach to consuming a nutrient-dense diet, supplementation and Vitamin D, and stress reduction. Discover food as medicine; it’s time to thrive.
Dr. Wahls Interview with Five to ThriveDr. Wahls and Chris Kresser, L. Ac Interview
Dr. Wahls sits with Chris Kresser, L. Ac to talk on Treating MS and Autoimmune Disease. <a href="https://chriskresser.com/treating-ms-and-autoimmune-disease-with-dr-terry-wahls/" target="_blank" >https://chriskresser.com/treating-ms-and-autoimmune-disease-with-dr-terry-wahls/</a>
Dr. Wahls and Chris Kresser, L. Ac InterviewDr. Wahls interviews with Multiple Sclerosis Radio

Dr. Terry Wahls is a physician, but is also a patient due to her personal journey with multiple sclerosis. Here, Dr. Wahls revisits Multiple Sclerosis Radio and shares her story as a patient and how over the last few years, her protocol for eating a nutrient dense diet has evolved <a herf="http://multiplesclerosisradio.com/the-wahls-protocol/" target="_blank">http://multiplesclerosisradio.com/the-wahls-protocol/</a>
Dr. Wahls interviews with Multiple Sclerosis RadioResearch Update-Full Edition

The Journal of Alternative and Complementary Medicine has published our paper, <strong>A Multimodal Intervention for Patients with Secondary Progressive Multiple Sclerosis: Feasibility and Effect on Fatigue,</strong> available <a href="https://pubmed.ncbi.nlm.nih.gov/24476345/" target="_blank">here.</a> The paper details the success of the first 10 subjects that we enrolled in the study, which uses diet, vitamins, stress reduction, exercise, and electrical stimulation of muscles to augment the effectiveness of the exercise program. Our study showed that intervention had very good compliance measures, is well tolerated, and has minimal side effects. In addition, the perceived fatigue was markedly reduced as compared to baseline fatigue levels. Group average fatigue severity (FSS) scores decreased from 5.7 at baseline to 3.32 (p=0.0008) at 12 months. We have not found any papers in the MS literature that report such a large favorable change on perceived fatigue. Such a large favorable change for fatigue is very exciting as fatigue is the most disabling symptom for those with MS and many other conditions.
Research Update-Full EditionAbstract - A Multimodal Intervention for Patients with Secondary Progressive Multiple Sclerosis: Feasibility and Effect on Fatigue

Below is the abstract of the recent published article: A Multimodal Intervention for Patients with Secondary Progressive Multiple Sclerosis: Feasibility and Effect on Fatigue published on <a href="https://pubmed.ncbi.nlm.nih.gov/24476345/" target="_blank">PubMed</a>.
Abstract - A Multimodal Intervention for Patients with Secondary Progressive Multiple Sclerosis: Feasibility and Effect on FatigueEarthing

For thousands of years, humans walked and slept directly on the ground. Today, we rarely walk barefoot outside. After reading <a href="https://www.amazon.com/Earthing-Most-Important-Health-Discovery/dp/1591202833/ref=dp_return_2?ie=UTF8&n=283155&s=books" target="_blank">Earthing: The Most Important Health Discovery Ever? (Paperback)</a> by Clinton Ober, Dr. Steven Sinatra, and Martin Zucker, I believe this disconnect with the earth could be a risk factor for poor health.
EarthingDr. Wahls Interview with Dr. Sarah Ballantyne (aka The Paleo Mom)

During this <a href="http://www.thepaleomom.com/2014/02/tpv-podcast-episode-79-dr-wahls.html" taget="_blank">interview</a>, Dr. Wahls speaks with Dr. Sarah Ballantyne, also known as The Paleo Mom.
Dr. Wahls Interview with Dr. Sarah Ballantyne (aka The Paleo Mom)Exercise and Brain Health

If you are like many Americans, your brain may be shrinking without your even knowing it. This is caused by a sedentary lifestyle that no longer promotes exercise and physical activity, both of which have a critical impact on the size of our brains. Exercise promotes the release of hormones in the brain called nerve […]
Exercise and Brain HealthDiane Bekel

I have the good fortune to have Dr. Wahls as a physician in the Polytrauma Clinic at the local VA. She outlined the diet, and I chose to give it a try. It’s not easy to stick to it–I fell away from my routine at Christmas. But I can tell the difference in my ability to think quickly and clearly when I follow the protocol as opposed to when I am eating the way I used to eat. For me, I am making a lifetime commitment to keeping the protocol going because the of the positive mental changes. – Diane Bekel, Iraq War Veteran
Diane BekelCreamy Cold Tomato Soup

Creamy Cold Tomato Soup Serves: 5 Ingredients 1 cucumber, chopped 1 scallion, chopped 1 clove garlic 4 cups tomato juice 1 green pepper, chopped ½ teaspoon dill weed 1 can full fat coconut milk Sliced mushrooms or tomato chunks for garnish Instructions Combine all ingredients in small amounts in blender and blend until smooth. Use […]
Creamy Cold Tomato SoupSweet and Savory Carrot Soup

I have made substitutions to make the recipe more consistent with what I would do.
Sweet and Savory Carrot SoupDo You Have an Autoimmune Problem?
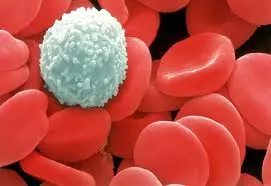
Autoimmunity, which is when our white blood cells treat parts of our bodies as foreign invaders and attack and destroythose necessary structures, is a big problem in America. Roughly 25 million Americans have an autoimmune diagnosis and another 50 million have auto-antibodies in their bloodstream but no clear diagnosis. The symptoms of autoimmunity often occur years or decades before a diagnosis is made. Meanwhile, our own bodies are eating away at themselves, damaging our brain, our joints, our skin, and even our blood vessels.
Do You Have an Autoimmune Problem?Stay Involved to Support the Foundation!

You can also support our work by sending the <a href="https://www.youtube.com/watch?v=KLjgBLwH3Wc" title="Terry Wahls' Tedx Talk" target="_blank">TEDx Talk link</a> to your friends and family or refer them to come to TheWahlsFoundation.com for more information. Please feel free to comment on the video on how eating the way your DNA expects — meaning following the Wahls Way™ — has helped you and your loved ones.
Stay Involved to Support the Foundation!The Healing Power of Color

As we age, our brains shrink, and that shrinkage progresses more rapidly for those with multiple sclerosis. In fact, anyone with high blood pressure, diabetes, or heart disease is also at a higher risk for brain shrinkage. Brain shrink occurs when brain cells die and are not replaced. As you can imagine, that is not a good thing — it is far better to help keep brain cells healthy, thus preventing their premature death. There is more and more research about the foods that help protect our brain cells from this premature dying. Antioxidant-rich vegetables and fruits are an important brain-maintaining food category we should eat everyday.
The Healing Power of Color
Dr. Terry Wahls is best known for her work in using diet and lifestyle interventions to manage MS, a condition she’s been diagnosed with herself. As a clinical professor, an author, and a speaker, she educates the public and medical community about the healing power of the Paleo diet and therapeutic lifestyle changes that improve the health and vitality of autoimmune, neurologic, and chronically diseased patients. Through her work, Dr. Wahls aims to shift the standard care for autoimmune patients and create an epidemic of health.
