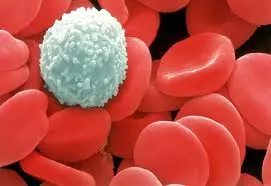
Some people are troubled by histamine intolerance. Histamine is produced and released by immune cells (mast cells and basophils).
Gut microbes also make histamine.
In addition, some foods also contain histamine.
Histamine induces the contraction of smooth muscles (bronchioles in the lungs and small intestine) and dilates blood vessels, increasing their leakiness. Histamine release can cause heart rhythm disturbance, change in blood pressure, increased mucus secretion (runny nose), and pain.
Symptoms that may arise from excessive activation of mast cells and release of histamine include:
- bloating
- skin rashes (flushing, hives, or eczema)
- itching
- runny nose
- increased tearing
- headaches
- diarrhea
- severe menstrual cramps
- and low blood pressure.1-3
Some may also experience:
- anxiety
- depression
- panic disorders
- sleep disturbance
- and severe fatigue.
Clinical diagnosis of mast cell activation and histamine sensitivity remains a challenge. There are hundreds of different mediators in mast cells, not just histamine. And the mediators that are released when mast cells are activated are quickly metabolized. That is why it is difficult to have a single blood test that can confirm mast cell activation or histamine sensitivity issues. Standardized testing is simply not available.
At present, other causes of the symptoms must be ruled out. Diagnosis requires at least two clinical symptoms that occur in less than four hours after eating high-histamine foods, and improvement in symptoms after adopting a low-histamine diet. A good response is a significant reduction in symptoms after 2 months of a low histamine diet.1,3
Foods high in histamine may trigger histamine-related symptoms.
High histamine foods include:
- citrus fruits
- strawberries
- bananas
- pineapple
- eggplant
- avocado
- tomatoes
- olives
- beans,
- canned meats
- smoked meats
- dried meats or fish
- yogurt
- cheese
- vinegar
- soy sauce
- fermented foods
- kimchi
- sauerkraut
- kombucha
- vinegar
- soy sauce
- beer,
- wine
- coffee
- and black tea.
In my clinical practice, I discuss the possibility that symptoms may be related to unrecognized gluten and casein sensitivity and direct patients to start with level one of the Wahls™ diet.
If they are still symptomatic after 3 months of the Wahls™ diet, I have the patient implement a low FODMAPS version of the Wahls™ diet. FODMAP (fermentable oligo-, di-, monosaccharides, and polyol) sensitivity may be the true cause of the symptoms.
Again the Wahls™ diet (level one) is often very helpful in reducing these types of symptoms, as is a low FODMAP version of the Wahls™ diet.
Eliminating legumes and reducing or eliminating onions, garlic, and fruit for six months can be very revealing.
The main dietary sources for the FODMAPS are:
- Oligosaccharides: wheat, rye, legumes, garlic, onions
- Disaccharides: milk, yogurt, cheese (lactose)
- Monosaccharides: honey, agave nectar, and fructose (fruit sugars)
- Polyols: blackberries, lychee
If symptoms persist, a trial of a low-histamine diet is in order.
The first step is freezing leftover foods; prolonged food storage increases histamine content.
Slow cooking also increases histamine levels in food, as does frying and grilling.
Boiling and steaming decrease histamine content.
Pressure cooking for a shorter time at high pressure does not increase histamine content.
Another strategy for managing histamine intolerance is to use Diamine Oxidase (DAO) to facilitate the breakdown of histamine in the gut.
Adding Diamine Oxidase has improved dietary tolerance of histamine and increased the ability of many patients to consume more histamine-rich foods. In a research study, adding supplemental DAO reduced histamine-related symptoms (rashes, headaches, blood pressure, abdominal complaints) and improved dietary tolerance of histamine-rich foods.1 Adding a DAO supplement has been helpful to my patients with histamine sensitivity, allowing them to follow a less restrictive diet.
If you believe you have histamine intolerance, I suggest you begin by adopting level one of the Wahls™ diet. If that is insufficient, reduce the FODMAP foods–onions, garlic, berries, and fruit sugars.
Consider a trial of a low histamine diet coupled with a DAO supplement.
After 6 months, you may slowly try adding back some higher histamine foods to assess if you can now tolerate a more moderate intake of histamine. Make dietary changes slowly to assess the impact of higher histamine foods. Often people are able to have a less restrictive diet when they also include DAO in their supplement routine.
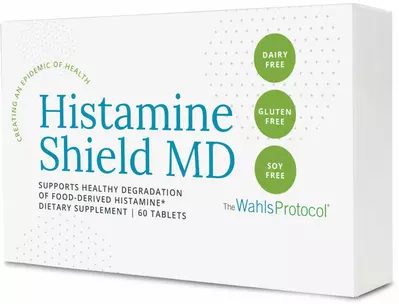 The Wahls Protocol® Histamine Shield is a patented enzyme formula containing diamine oxidase (DAO)—the main enzyme responsible for the degradation of ingested histamine. This enzyme has been clinically tested and found to break down food-derived histamine in the digestive tract. DAO is not absorbed and does not have systemic activity.
The Wahls Protocol® Histamine Shield is a patented enzyme formula containing diamine oxidase (DAO)—the main enzyme responsible for the degradation of ingested histamine. This enzyme has been clinically tested and found to break down food-derived histamine in the digestive tract. DAO is not absorbed and does not have systemic activity.
Save 10% off your first order using code WAHLS10
References:
Comas-Baste O,Sanchez-Perez S, Veciana-Nogues MT, Latorre-Moratalla M, Vidal-Carou MDC. Histamine Intolerance: The Current State of the Art. *Biomolecules.*>2020;10(8).
Fogel WA, Lewinski A, Jochem J. Histamine in food: is there anything to worry about? *Biochem Soc Trans.* 2007;35(Pt 2):349-352.
Smolinska S, Winiarska E, Globinska A, Jutel M. Histamine: A Mediator of Intestinal Disorders-A Review.*Metabolites.*2022;12(10).