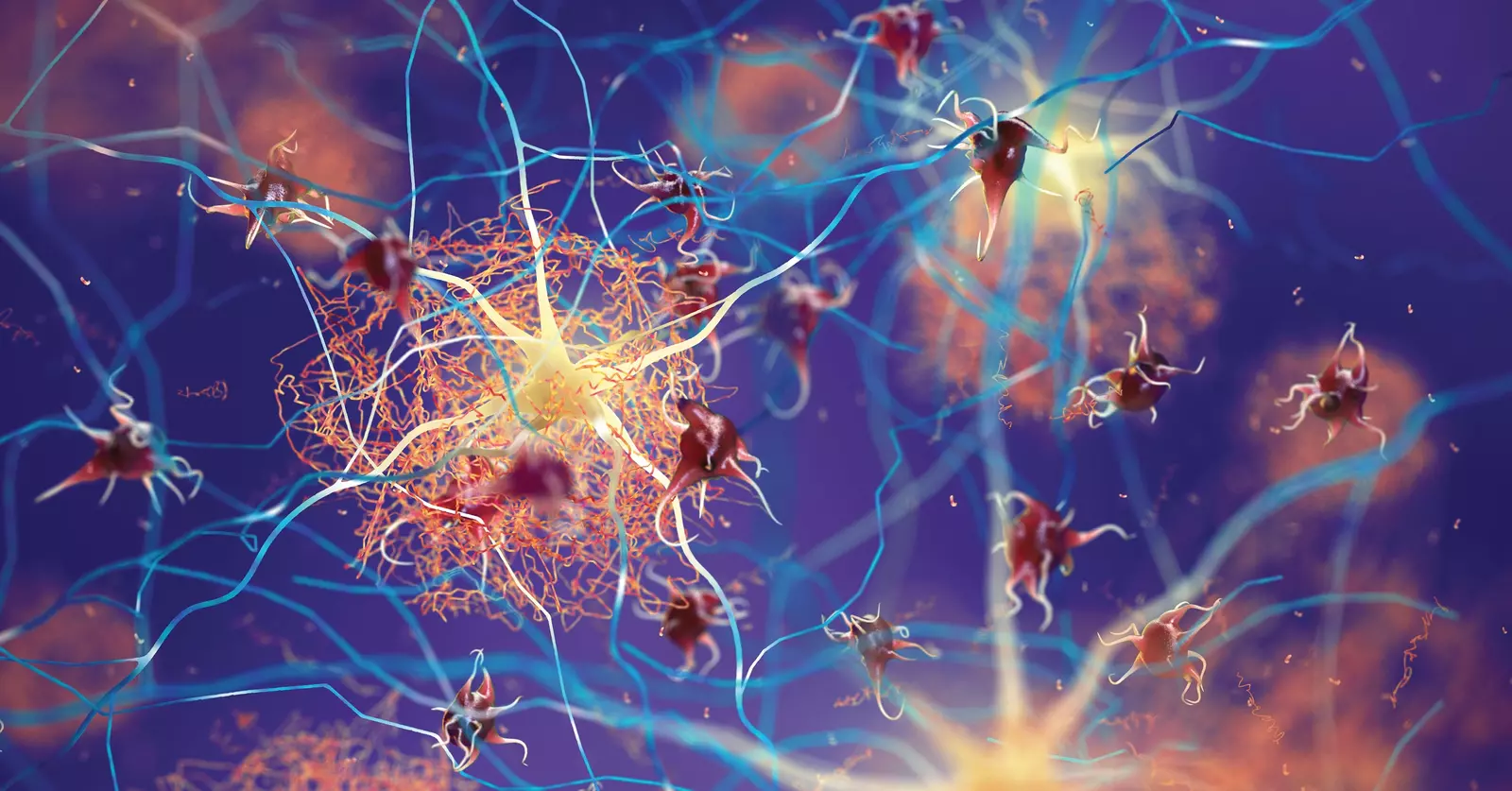
Most of us want to stay healthy as we age and be able to repair any damage that occurs to our central nervous system, that is our brain and spinal cord. Microglia and astrocytes play a big role in that process1,2. They provide structure and support for the neurons, the brain cells that receive signals from our sensory organs and send signals to our muscles. Astrocytes are also important for the blood-brain barrier, providing nutrients and oxygen to our neurons. Microglia are the immune cells of the central nervous system. Depending on the microenvironment, your microglia and astrocytes may be healing your brain or creating more damage, which can lead to more disease and rapid aging.
Astrocytes and microglia are continuously inspecting the environment for signs of safety and danger. Protein fragments that match bacterial proteins are danger signals that trigger the immune system to react and attack. LPS or lipopolysaccharide protein fragments are especially strong danger signals to our immune cells. Signals of cell damage are also strong danger signals. Protein fragments that are supposed to be inside the cells become danger signals if these protein fragments spill outside the cell. One example of such a compound is adenosine triphosphate or ATP. Inside the cell, ATP carries energy and helps facilitate the biochemistry of life. Outside the cell, however, ATP becomes a potent danger signal, telling the body there is a threat and activating immune cells, which then produce pro-inflammation cytokine molecules to phagocyte (or dissolve) the damaged cells.
Having more LPS enter the bloodstream because of a leaky gut increases the probability that some of the LPS will also cross the blood-brain barrier. If the LPS is detected by the microglia in the central nervous system, the microglia will shift from the patrolling state (M0) to the reactive state (M1). In the M1 state, the microglia increase the production of pro-inflammation cytokines in the brain and begin eating up synapses, damaging the oligodendrocytes (myelin-producing cells) and neurons. When the microenvironment is less threatening, the microglia shift to a less reactive M2 state, which promotes repair of synapses and myelin3. There is complicated interplay between microglia, astrocytes, and the microenvironment that determines the response to the danger signal and the return to a reparative state.
There are considerable efforts to find drugs that will shift the microglia away from the danger response. However, because of the complexities of feedback loops on sensing danger and safety in the central nervous system3, I predict there will be great difficulty in finding drugs that can safely shift microglia away from the danger response.
Instead, we should be focused on creating a microenvironment that favors safety and lowers the danger signal. Strategies for lowering the reactivity of microglia include improved sleep4, improved nutrition4,6, and exercise4,6. People with autoimmune conditions are likely to have increased intestinal permeability, which increases the risk of LPS crossing into the bloodstream and entering the central nervous system7. It also increases the likelihood of a leaky blood-brain barrier. Unrecognized gluten sensitivity is common in those with an autoimmune disorder with central nervous system involvement8. Improving the microenvironment starts with an elimination diet to remove the most common food sensitivities (gluten, dairy, and eggs) or food sensitivity testing to identify foods that may be causing an immune response. For anyone with a neurologic or psychiatric issue who likely has reactive microglia, a trial of a gluten-free diet is warranted.
Other dietary strategies that may improve the microenvironment include reducing added sugars, increasing intake of fiber, and eating more fermented foods to increase microbiome diversity4,9,10. A variety of dietary patterns would likely help reduce danger signals in the central nervous system: Mediterranean diet, Paleolithic diet, nutrient-dense vegetarian diet, or a nutrient-dense ketogenic diet. Improved cellular health starts with reducing added sugar, high–glycemic index foods (pasta, white bread, whipped white potatoes, and sugary beverages) and processed foods.
There are non-dietary lifestyle factors that can also reduce microglia reactivity, including improving sleep quality and quantity. How many hours of sleep do you get each night? Do you feel rested and refreshed in the morning? Do you snore? Reducing exposure to ultraviolet lights from phones, computers, artificial lights, and televisions in the evening can assist with the production of melatonin, the hormone that facilitates falling asleep. Getting outside in the sunlight during the day can improve the circadian rhythm, timing of cortisol and melatonin, and sleep quality and quantity11.
If you have a neurological or psychiatric illness, you likely have microglia that are overly reactive. Healthy aging starts with microglia that are reparative rather than damaging. Diet and lifestyle choices can reduce the danger signals in the microenvironment. I have been teaching these concepts since 2008 when I began sharing the Wahls Protocol® with the public. Now we are beginning to understand the molecular processes that explain why the Wahls Protocol® is so successful at reducing pain and fatigue and improving mood and mental clarity in so many different disease states. The Wahls Protocol® is likely reducing the reactivity of the microglia, shifting the body towards the reparative M2 function of the microglia and, as healing is completed, returning the microglia to M0, the patrolling state.
If you have a neurological or psychiatric disease state, using diet and lifestyle to shift your microglia should be a key part of your self-care. If you need more help implementing and sustaining your self-care program, sign up for the autoimmune intervention mastery course, an online course with short digestible lessons to teach you what diet and lifestyle choices will improve your health and offer support as you progress on your healing journey.
References:
Domingues HS, Portugal CC, Socodato R, Relvas JB. Oligodendrocyte, Astrocyte, and Microglia Crosstalk in Myelin Development, Damage, and Repair. *Front Cell Dev Biol.* 2016;4:71.
Wolf SA, Boddeke HW, Kettenmann H. Microglia in Physiology and Disease. *Annu Rev Physiol.* 2017;79:619-643.
Mesquida-Veny F, Del Rio JA, Hervera A. Macrophagic and microglial complexity after neuronal injury. *Prog Neurobiol.* 2021;200:101970.
Muscat SM, Barrientos RM. Lifestyle modifications with anti-neuroinflammatory benefits in the aging population. *Exp Gerontol.* 2020;142:111144.
Madore C, Yin Z, Leibowitz J, Butovsky O. Microglia, Lifestyle Stress, and Neurodegeneration. *Immunity.* 2020;52(2):222-240.
Nijs J, Tumkaya Yilmaz S, Elma O, et al. Nutritional intervention in chronic pain: an innovative way of targeting central nervous system sensitization? *Expert Opin Ther Targets.* 2020;24(8):793-803.
Obrenovich MEM. Leaky Gut, Leaky Brain? *Microorganisms.* 2018;6(4).
Antonini M, Lo Conte M, Sorini C, Falcone M. How the Interplay Between the Commensal Microbiota, Gut Barrier Integrity, and Mucosal Immunity Regulates Brain Autoimmunity. *Front Immunol.* 2019;10:1937.
Duggan MR, Parikh V. Microglia and modifiable life factors: Potential contributions to cognitive resilience in aging. *Behav Brain Res.* 2021;405:113207.
McKenzie JA, Spielman LJ, Pointer CB, et al. Neuroinflammation as a Common Mechanism Associated with the Modifiable Risk Factors for Alzheimer’s and Parkinson’s Diseases. *Curr Aging Sci.* 2017;10(3):158-176.
11. Zhao ZC, Zhou Y, Tan G, Li J. Research progress about the effect and prevention of blue light on eyes. *Int J Ophthalmol.* 2018;11(12):1999-2003.