The major trouble with finding blood on your toothbrush—bleeding gums are a signal that something is wrong.
A little bit of blood on your toothbrush after brushing or flossing your teeth may feel normal, but it’s not healthy.
Unless you have actually cut your gums, bleeding is a sign of infection. Your gums should never bleed. Think about your fingernails. If you were scrubbing your nails with a scrub brush, it wouldn’t be normal for them to bleed, would it?
If you are experiencing bloody gums after brushing or flossing, you likely have gum disease (periodontitis) caused by bacteria in your mouth. This has the potential to cause trouble on many fronts.
Before we discuss the bad stuff, let’s talk about the good stuff.
The bacteria in our mouths form a biofilm of dental plaque that is part of the oral microbiome. The balance of bacteria impacts the whole body’s ability to create health.
Dental plaque has a purpose. In a perfect environment:
- it serves as the gatekeeper to the minerals in saliva and can help put minerals back into the tooth surface as needed.
- it can provide a shield that keeps bad actors from getting into the gum-tooth space.
- it becomes a chemical buffer to maintain a normal pH level that allows teeth and gums to thrive.
Additionally, the good bacteria in the mouth contribute to the conversion of dietary nitrates to nitrites, which improve blood vessel health and blood pressure.(1)
Dental plaque becomes problematic when the biofilm becomes protection for undesirable organisms, shielding them from the immune system and antimicrobials that would otherwise eliminate them. Plaque can create an environment where a variety of microbial species can support each other and multiply.
These bad organisms include gram negatives and more serious pathogens, such as porphyromonas gingivalis (P. Gingivalis). The presence of periodontitis is associated with a higher risk of developing atherosclerosis (2), metabolic syndrome(3), diabetes<sup(4), and respiratory diseases.(5)
If oral film builds up, pathogenic bacteria in the mouth (P. Gingivalis in particular) increase in number and become more virulent. Presence of P. Gingivalis in the mouth is associated with higher levels of systemic inflammation and increased risk of a wide variety diseases including cancer, chronic heart infections (endocarditis), and rheumatoid arthritis.(6) In addition, P. Gingivalis increases the risk of Alzheimer’s disease and neurodegeneration.(7)
The buildup of dental plaque increases the circulation of gram negative bacteria, including P. Gingivalis, and bacterial molecules like lipopolysaccharides (LPS) and flagellin. These molecules enter the bloodstream and increase the production of inflammatory cytokines and leakiness of both the intestinal barrier and the blood-brain barrier.
The increased leakiness of the gut and brain barriers leads to increased production of inflammation-producing cytokines and more reactive immune cells (THh17). In the brain, increased cytokines lead to reactive microglia, which are the brain’s immune cells.
The microglia produce more cytokines, which activate the innate immune system and lead to damaged connections between brain cells (synapses), damage to the insulation around the wiring between brain cells (myelin), and damage to the brain cells (neurons), all of which increase the risk of neurological and psychiatric diseases.(8,9)
Traditional approaches to reducing the risk of periodontitis have focused on brushing and flossing with periodic removal of the plaque buildup by a dental hygienist. As we understand more and more about how the oral biome interacts with other biochemical conversations within the body, conventional dentists are slowly starting to adopt a functional medicine approach to patient care.
Biological dentists treat the whole health of the patient and emphasize prevention and conservative treatment methods. Utilizing lifestyle changes and non-pharmaceutical treatments, biological dentists can help you prevent diseases from developing or progressing. They also treat less understood systemic diseases rooted in poor oral health.
There is more recent recognition of the benefit of increased consumption of non-starchy vegetables, sufficient protein, and diet quality on the risk of periodontitis.(10,11) Probiotics and nutraceuticals are also beneficial for improving the number of good bacteria and reducing the number of bad bacteria in the mouth.(12,13)
My approach to maintaining a healthy oral biome:
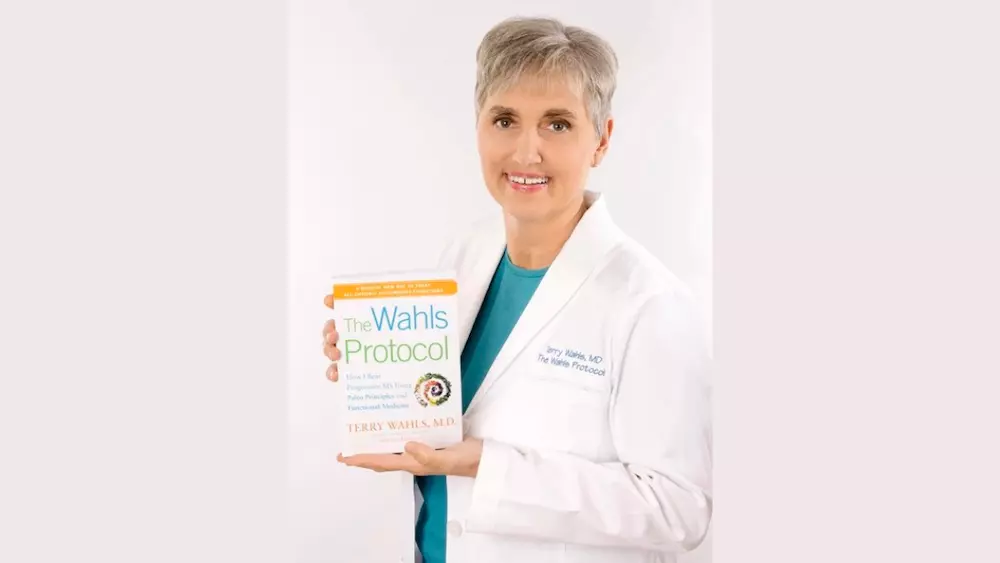
I see a biological dentist twice a year and each visit he tells me that my teeth and gums are incredibly healthy. Of course, I follow the Wahls Protocol® and consume a relatively low carbohydrate diet, avoiding simple starches and fructose-based sweeteners.
I brush and floss my teeth twice daily, and often swish coconut or sesame oil in my mouth for a few minutes to reap the benefits of oil pulling. I also regularly brush with activated charcoal to help pull toxins from the mouth and remove stains.
Sourcing a quality toothpaste can be a challenge but I have found that Wellnesse has toothpaste products that are strategically formulated to support a healthy oral biome and help remineralize teeth.
Some of my favorites are:
The Whitening Toothpaste is a one-stop shop featuring ingredients like:
- Aloe vera to eliminate disease-causing bacteria, whiten teeth, and reduce staining,
- Green tea powder to help combat bad breath,
- Hydroxyapatite, which restores enamel and helps remineralize teeth,
- Peppermint oil, which is antimicrobial and antiviral,
- and Neem oil, which prevents tooth decay and gum disease.
The Charcoal Toothpaste —use a few times a week to strengthen, whiten, and detoxify your smile.
Your oral health and overall health are inextricably linked, which is why it is so important to make your oral biome a top priority in your self-care routine. If you are ready to restock your bathroom cabinet, check out wellnesse.com for eco-friendly oral and personal care offerings.
Looking for a unique holiday gift?
Save up to 25% OFF when you use this link.
I do want to let you know that the team at terrywahls.com does receive a small affiliate commission for any product ordered through Wellnesse. This is part of how we are able to produce so many informational resources at no cost to you. If you’re not comfortable with an affiliate link—no worries, I hope that you do find the information shared to be beneficial!
References:
Alzahrani HS, Jackson KG, Hobbs DA, Lovegrove JA. The role of dietary nitrate and the oral microbiome on blood pressure and vascular tone. *Nutr Res Rev.* 2021;34(2):222-239.
Almeida A, Fagundes NCF, Maia LC, Lima RR. Is there an Association Between Periodontitis and Atherosclerosis in Adults? A Systematic Review. *Curr Vasc Pharmacol.* 2018;16(6):569-582.
Gurav AN. The association of periodontitis and metabolic syndrome. *Dent Res J (Isfahan).* 2014;11(1):1-10.
Baeza M, Morales A, Cisterna C, et al. Effect of periodontal treatment in patients with periodontitis and diabetes: systematic review and meta-analysis. *J Appl Oral Sci.* 2020;28:e20190248.
Pathak JL, Yan Y, Zhang Q, Wang L, Ge L. The role of oral microbiome in respiratory health and diseases. *Respir Med.* 2021;185:106475.
Kriebel K, Hieke C, Muller-Hilke B, Nakata M, Kreikemeyer B. Oral Biofilms from Symbiotic to Pathogenic Interactions and Associated Disease -Connection of Periodontitis and Rheumatic Arthritis by Peptidylarginine Deiminase. *Front Microbiol.* 2018;9:53.
Pritchard AB, Crean S, Olsen I, Singhrao SK. Periodontitis, Microbiomes and their Role in Alzheimer’s Disease. *Front Aging Neurosci.* 2017;9:336.
Feres M, Teles F, Teles R, Figueiredo LC, Faveri M. The subgingival periodontal microbiota of the aging mouth. *Periodontol 2000.* 2016;72(1):30-53.
Meghil MM, Cutler CW. Oral Microbes and Mucosal Dendritic Cells, “Spark and Flame” of Local and Distant Inflammatory Diseases. *Int J Mol Sci.* 2020;21(5).
Gondivkar SM, Gadbail AR, Gondivkar RS, et al. Nutrition and oral health. *Dis Mon.* 2019;65(6):147-154.
Rowinska I, Szyperska-Slaska A, Zariczny P, Paslawski R, Kramkowski K, Kowalczyk P. The Influence of Diet on Oxidative Stress and Inflammation Induced by Bacterial Biofilms in the Human Oral Cavity. *Materials (Basel).* 2021;14(6).
Isola G. Current Evidence of Natural Agents in Oral and Periodontal Health. *Nutrients.* 2020;12(2).
13. Isola G. The Impact of Diet, Nutrition and Nutraceuticals on Oral and Periodontal Health. *Nutrients.* 2020;12(9).